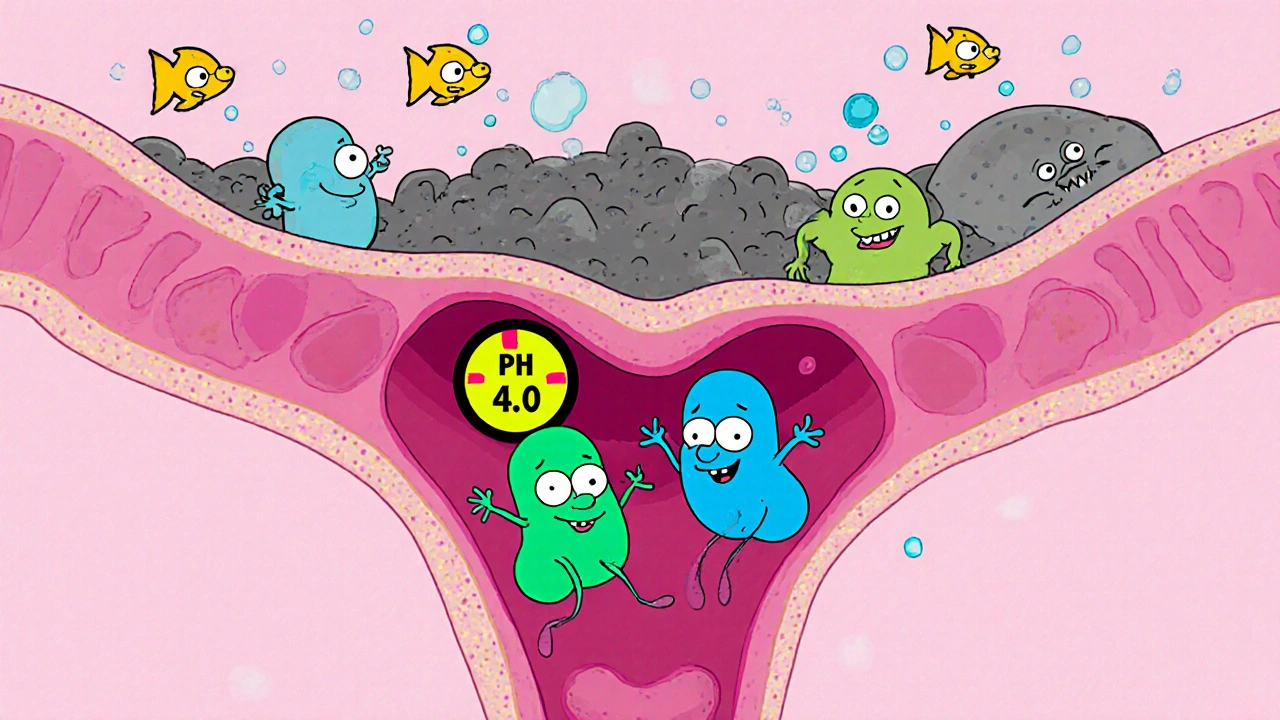
Bacterial Vaginosis is a common vaginal infection caused by an imbalance of the normal flora, particularly a reduction in Lactobacillus species and an overgrowth of anaerobic bacteria. When the pH shifts above its usual 3.8-4.5 range, symptoms like thin grayish discharge, fishy odor, and mild itching can appear. Vaginal Dryness often shows up alongside BV, especially after treatment or during hormonal fluctuations, leaving many women wondering if the two are linked and how to find relief.
Understanding the Connection Between BV and Dryness
Even though BV and dryness seem like opposite problems-one is excess fluid, the other a lack of moisture-they share underlying mechanisms:
- Microbial imbalance: A drop in protective Lactobacillus reduces natural secretions that keep the vaginal lining supple.
- Inflammation: Inflammatory responses to bacterial overgrowth can damage the epithelial cells that produce mucus.
- Treatment side‑effects: Antibiotics such as Metronidazole or Clindamycin kill both harmful and beneficial bacteria, sometimes leaving the lining dry.
- Hormonal shifts: Menstrual cycle, menopause, or hormonal contraceptives affect both pH and lubrication.
Recognising these links helps you target relief more precisely rather than just masking symptoms.
Self‑Assessment: Spotting Symptoms Early
Before you reach for a product, ask yourself these quick questions:
- Do you notice a thin, gray‑white discharge with a distinct fishy smell?
- Is there a burning sensation during urination or intercourse?
- Has your vagina felt unusually dry, flaky, or uncomfortable after sex?
- Have you recently completed a course of antibiotics for BV?
If you answered yes to two or more, it’s worth confirming BV with a healthcare provider. A simple microscope exam looking for "clue cells" can diagnose the condition in minutes.
When to See a Health Professional
Home care works for mild cases, but professional help is essential if:
- Symptoms persist for more than a week after treatment.
- You experience pelvic pain, fever, or unusual bleeding.
- You’re pregnant-BV can increase the risk of preterm birth.
- You have recurrent episodes (three or more in a year).
Doctors may prescribe a repeat antibiotic course, a probiotic regimen, or, in rare cases, a topical estrogen cream to restore moisture.

Evidence‑Based Relief Strategies
Below are practical steps you can start today. Each approach tackles a different part of the problem-microbial balance, pH regulation, and lubrication.
1. Re‑Establish Healthy Flora
- Probiotic supplements: Look for strains like Lactobacillus rhamnosus GR‑1 and Lactobacillus reuteri RC‑14. Clinical trials in 2023 showed a 30% reduction in BV recurrence when taken daily for three months.
- Fermented foods: Yogurt with live cultures, kefir, and sauerkraut can seed your gut with helpful bacteria that travel to the vaginal area.
- Avoid douching: It disrupts the natural balance and can worsen both BV and dryness.
2. Keep pH in Check
- pH‑balanced washes: Products labeled “pH 3.8‑4.5” help maintain the acidic environment without stripping moisture.
- Apple cider vinegar rinse: Dilute one tablespoon in a cup of warm water and use as a gentle vaginal soak once a week. Studies show a modest drop in pH after four weeks.
3. Moisturize the Vaginal Tissue
Choose the right type based on frequency of use and personal preference. The table below compares the most common over‑the‑counter options.
| Product Type | Key Ingredients | Duration of Relief | Best For | Potential Irritants |
|---|---|---|---|---|
| Water‑Based Lubricant | Glycerin, Propylene Glycol | 1-2 hours | Spontaneous sex, occasional use | Glycerin (may feed yeast) |
| Silicone‑Based Lubricant | Dimethicone, Cyclomethicone | 3-4 hours | Longer sessions, water‑play | Rare, but can leave a residue |
| Vaginal Moisturizer (gel) | Hydroxyethylcellulose, Aloe Vera | Up to 48 hours | Daily comfort, chronic dryness | Fragrance (if added) |
| Estrogen Cream (prescription) | Estradiol | Weeks to months | Post‑menopausal dryness | Not recommended for BV without doctor approval |
For most women dealing with BV‑related dryness, a daily gel moisturizer topped with a water‑based lubricant for sexual activity works well. Avoid products with high glycerin or parabens if you have a history of yeast infections.
4. Lifestyle Tweaks That Help
- Stay hydrated: Adequate water intake supports overall mucosal health.
- Wear breathable underwear: Cotton allows airflow, reducing irritation.
- Manage stress: Cortisol spikes can alter hormone levels and affect vaginal secretions.
- Limit sugary foods: High sugar can promote yeast overgrowth, compounding discomfort.
5. Sexual Activity Considerations
Sex can temporarily worsen dryness, but communication with your partner helps. Try these tips:
- Apply a small amount of lubricant 10 minutes before intercourse.
- Use condoms made of latex‑free materials if you’re sensitive to latex.
- Engage in longer foreplay to stimulate natural lubrication.
Putting It All Together: A Daily Relief Routine
- Morning: Take a probiotic capsule (containing L. rhamnosus GR‑1 and L. reuteri RC‑14). Follow with a cup of plain yogurt.
- Mid‑day: If you feel dryness, apply a thin layer of a hyaluronic‑acid‑based vaginal gel.
- Evening: Perform a gentle pH‑balanced wash. Rinse with a diluted apple cider vinegar solution once a week.
- Before intimacy: Apply a water‑based lubricant, reapply as needed.
- Weekly: Review any changes; note if discharge or odor returns, and schedule a check‑up if needed.
This routine addresses both the root cause (microbial imbalance) and the symptom (dryness) without over‑relying on prescription meds.

Common Myths Debunked
- Myth: “If I’m dry, I can’t have BV.”
Fact: BV can coexist with dryness; the infection often reduces natural lubrication. - Myth: “Douching cleanses the vagina.”
Fact: It strips protective bacteria and can trigger both BV and dryness. - Myth: “All lubricants are safe.”
Fact: Glycerin‑rich lubricants may feed yeast, worsening irritation.
Quick Checklist for Relief
- Confirm BV diagnosis with a clinician.
- Start a daily probiotic regimen.
- Choose a pH‑balanced, fragrance‑free wash.
- Apply a long‑lasting vaginal moisturizer.
- Use a compatible lubricant during sex.
- Track symptoms for at least two weeks.
- Seek medical advice if symptoms persist or worsen.
Frequently Asked Questions
Can BV cause permanent vaginal dryness?
BV itself usually doesn’t cause permanent dryness. The condition can temporarily reduce natural secretions, but once the microbial balance is restored-often with probiotics and proper treatment-lubrication typically returns to normal.
Is it safe to use over‑the‑counter moisturizers while taking antibiotics for BV?
Yes, most OTC moisturizers are safe. Choose fragrance‑free, water‑based gels without glycerin if you’re prone to yeast. They won’t interfere with antibiotics, but they also won’t treat the infection.
How long should I wait after finishing antibiotics before trying a probiotic?
You can start a probiotic at the same time you begin antibiotics. Some studies show concurrent use helps maintain vaginal flora. If you experience severe side effects, wait until the antibiotic course ends and then start the probiotic for a month.
Are silicone lubricants better than water‑based ones for BV‑related dryness?
Silicone lubricants last longer and don’t contain glycerin, which can feed yeast. They’re a good choice if you have frequent dryness. However, they can be harder to clean from fabrics and may leave a residue, so a small amount before intimacy is recommended.
When should I consider prescription estrogen cream?
If you’re post‑menopausal, have chronic dryness, and have tried OTC options without relief, a low‑dose estrogen cream prescribed by a gynecologist can rebuild the vaginal lining. It’s not a first‑line treatment for BV, but it can complement antibiotic therapy.
By blending medical treatment with everyday self‑care-probiotics, pH‑balanced hygiene, and the right moisturizer-you can break the cycle of BV and vaginal dryness. Keep an eye on your body, stay consistent with the routine, and don’t hesitate to get professional guidance when needed.

Ericka Suarez
October 21, 2025 AT 01:15Look, I’m sick of all this nonsense about probiotics being a magic cure. The truth is that most of these "experts" are just selling you overpriced creams while the govment pretends everything’s fine. It’s a sham that our culture lets slide, and we keep swallowing the hype like it’s gospel. Stop trusting the mainstream and demand real science.
parbat parbatzapada
October 21, 2025 AT 03:26Honestly it feels like they’re hiding something bigger, like they don’t want us to see the real side effects. I can’t trust a system that markets comfort while pulling the strings behind the scenes.
Casey Cloud
October 21, 2025 AT 07:36Probiotic supplements that contain Lactobacillus rhamnosus GR‑1 and Lactobacillus reuteri RC‑14 have been studied in several trials and they show promise in reducing recurrence of BV. The strains work by recolonizing the vaginal flora and restoring the acidic pH that keeps harmful bacteria at bay. You can find these strains in oral capsules or in some vaginal suppositories. Taking a daily capsule for at least three months is a common recommendation. Consistency is key because the bacteria need time to establish themselves in the ecosystem. Pairing the probiotic with a diet that includes yogurt kefir and other fermented foods can boost the effect. Fermented foods deliver live cultures that travel through the gut and eventually reach the vaginal area. Avoid douching because it strips away the protective biofilm and sets back any progress you make. When you use a pH‑balanced wash you help keep the environment hostile to anaerobes while still being gentle on tissue. A diluted apple cider vinegar rinse once a week can lower the pH slightly and may help keep BV at bay if used correctly. For lubrication, a water‑based lubricant without glycerin is a safe choice for most women and it won’t feed yeast. If you need longer lasting relief silicone lubricants are an option but make sure they’re free of fragrances. For chronic dryness a vaginal gel with hyaluronic acid can provide moisture for up to two days. Stay hydrated throughout the day because overall fluid intake supports mucosal health. Remember that stress management also plays a role because cortisol can affect hormone balance. Finally keep an eye on any changes in discharge odor or texture and schedule a follow‑up with your provider if symptoms persist beyond two weeks.
Rachel Valderrama
October 21, 2025 AT 09:00Oh wow, thanks for the novel-now I can read a whole textbook before bedtime.
Eryn Wells
October 21, 2025 AT 13:10Hey folks! 🌟 Remember that every body is different so what works for one might not work for another. Let’s keep sharing our experiences and support each other on this journey. 💬
Kathrynne Krause
October 21, 2025 AT 14:33Absolutely love the vibe here-let’s sprinkle some glitter on the science and keep the convo lively.
Devendra Tripathi
October 21, 2025 AT 18:43Honestly most of these “evidence‑based” tips are just marketing fluff wrapped in clinical jargon.
Vivian Annastasia
October 21, 2025 AT 20:06Sure, because ignoring all research has always solved health problems, right?
Nick M
October 22, 2025 AT 00:16Big pharma loves the probiotic hype it’s just a cash grab.
eric smith
October 22, 2025 AT 01:40Actually the data isn’t a cash grab; the meta‑analysis shows a modest benefit, but you wouldn’t know that from your scrolling.
Erika Thonn
October 22, 2025 AT 05:50Life is a river of acidity and balance we must navigate with mindful intention, even in the intimate chambers of our being.
Jake Hayes
October 22, 2025 AT 07:13Balance is key; follow evidence, not poetry.
Brandy Eichberger
October 22, 2025 AT 11:23Thanks for the solid rundown, really helpful!