Diabetic retinopathy isn’t just a complication of diabetes-it’s the leading cause of preventable vision loss in adults under 65. Left unchecked, it can steal sight quietly, often without pain or warning. But here’s the good news: if caught early, diabetic retinopathy can be managed so effectively that up to 98% of severe vision loss can be avoided. The key isn’t just knowing you have diabetes-it’s knowing when and how often to get your eyes checked, and what happens if problems are found.
How Diabetic Retinopathy Develops
High blood sugar over time damages the tiny blood vessels in the retina-the light-sensitive layer at the back of your eye. These vessels can leak fluid, swell, or close off completely. In advanced stages, the eye tries to grow new blood vessels to compensate, but these are fragile and prone to bleeding, which can scar the retina or trigger retinal detachment.
The progression isn’t sudden. It usually takes years. That’s why regular screening matters so much. The condition is split into two main phases: nonproliferative diabetic retinopathy (NPDR), where vessels are damaged but not yet growing abnormally, and proliferative diabetic retinopathy (PDR), where new, unstable vessels form. Diabetic macular edema (DME), a swelling in the central part of the retina, can occur at any stage and is the most common reason for vision loss.
According to the International Diabetes Federation, about 103 million people with diabetes worldwide have some form of retinopathy. In Australia, where around 1.3 million people live with diabetes, this translates to roughly 1 in 3 adults with diabetes showing early signs.
Who Needs Screening and When
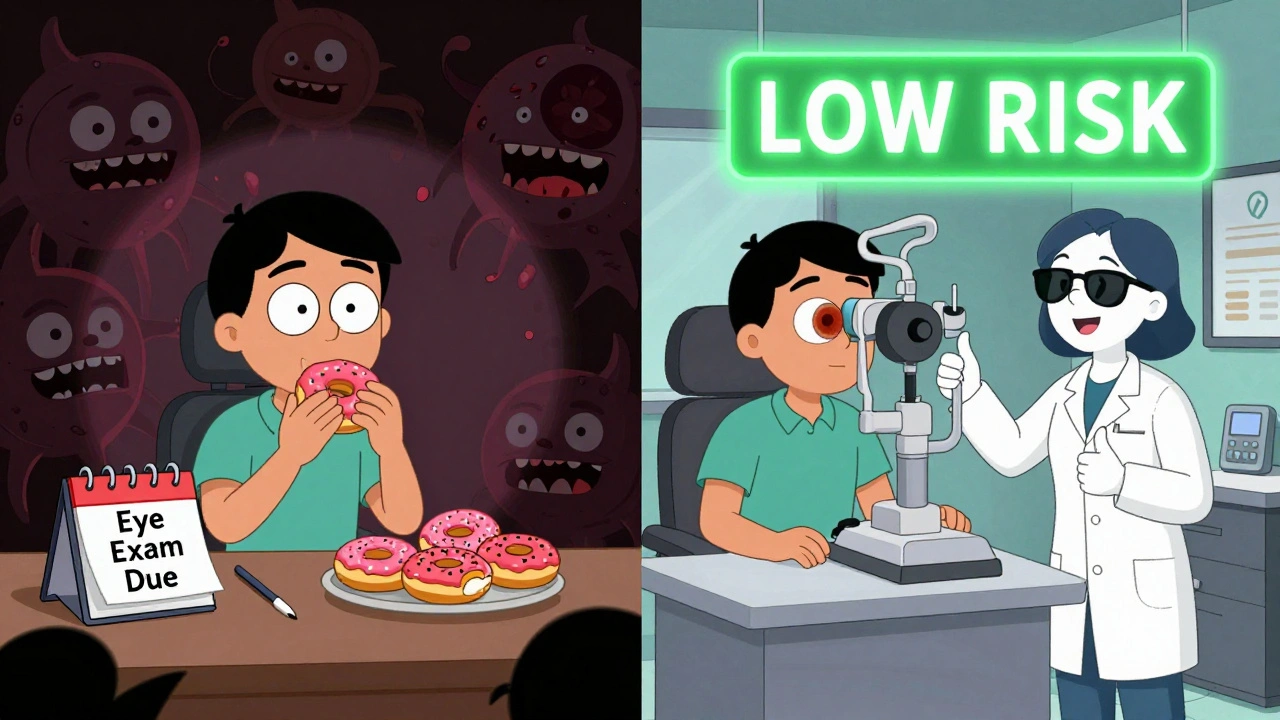
Screening isn’t one-size-fits-all. Your risk level determines how often you need an eye exam. The old rule-annual screening for everyone-is being replaced by smarter, risk-based schedules.
- If you have type 1 diabetes: Get your first eye exam 3-5 years after diagnosis, then follow up based on results.
- If you have type 2 diabetes: Get your first exam soon after diagnosis, since retinopathy may already be present.
After the first exam, your screening interval depends on what the doctor finds:
- No retinopathy or mild NPDR: Every 1-2 years is safe for most people, especially if your HbA1c is under 7%, your blood pressure is controlled, and you have no kidney damage.
- Moderate NPDR: You need to see an eye specialist every 3-6 months. This is the stage where early treatment can still prevent serious damage.
- Severe NPDR: You must be evaluated within 3 months. The risk of turning into PDR jumps significantly here.
- Proliferative DR or DME: You need to see a specialist within 1 month. Delaying treatment can mean permanent vision loss.
There’s also a tool called RetinaRisk that uses your HbA1c, diabetes duration, blood pressure, and kidney function to calculate your personal risk. Studies show it can cut unnecessary screenings by nearly 60% without missing cases. For example, someone with type 2 diabetes, HbA1c of 6.8%, no kidney issues, and 5 years of diabetes might only need screening every 4 years. But someone with HbA1c over 9% and high blood pressure might need checks every 6 months-even if they have no visible damage yet.
What Happens During a Screening
A diabetic eye screening isn’t just a quick glance. It’s a detailed digital photograph of your retina, taken after your pupils are dilated. This is called mydriatic fundus photography. Two images are taken of each eye, covering the central and outer retina. The goal? To spot even the smallest leaks, swelling, or abnormal blood vessels.
In many clinics now, artificial intelligence helps analyze the images. Google’s DeepMind algorithm, for example, detects sight-threatening retinopathy with over 94% accuracy-matching or beating human graders. In rural areas where ophthalmologists are scarce, telemedicine platforms send these images to specialists remotely. One study found these systems catch 94% of cases that need urgent care.
Some newer tools, like the D-Eye smartphone adapter, let primary care providers take retinal photos right in their office. It’s not perfect yet, but it’s 89% accurate compared to specialist readings-and it’s making screening possible for people who can’t get to an eye clinic.
Treatment Options: From Mild to Severe
Not every case needs surgery or injections. Treatment depends on how far the disease has gone.
- No or mild retinopathy: Focus on controlling blood sugar, blood pressure, and cholesterol. Studies show that lowering HbA1c from 9% to 7% can reduce retinopathy progression by over 50%. Lifestyle changes-diet, exercise, weight loss-are your first line of defense.
- Moderate to severe NPDR: Your doctor may recommend laser treatment (focal or panretinal photocoagulation) to seal leaking vessels and stop new ones from forming. This doesn’t restore vision but prevents further loss.
- Diabetic macular edema (DME): The most common cause of vision loss in diabetics. Treatment usually starts with anti-VEGF injections (like aflibercept or ranibizumab). These drugs block a protein that causes swelling and leaky vessels. Most patients get 3-6 injections in the first year, then maintenance doses every 2-4 months. Studies show over 90% of patients stabilize or improve vision with this approach.
- Proliferative DR: If new blood vessels are growing, you’ll likely need panretinal photocoagulation (PRP) laser therapy. In some cases, a vitrectomy (surgery to remove blood or scar tissue from the eye) is needed if bleeding doesn’t clear on its own.
It’s important to know: treatment doesn’t cure diabetic retinopathy. It stops it from getting worse. That’s why ongoing management is critical-even after treatment.
Why Skipping Screenings Is Risky
Some patients avoid screenings because they feel fine. Others are overwhelmed by appointments. But here’s the truth: diabetic retinopathy doesn’t hurt until it’s advanced. By the time you notice blurry vision, it’s often too late for full recovery.
One Reddit user, "RetinaScared2023," shared that their clinic pushed for 2-year screenings despite an HbA1c of 8.5%. Within 18 months, they developed macular edema. "I could’ve saved my vision if they’d just listened to my numbers," they wrote.
On the flip side, another user, "Type1Warrior87," said switching from annual to biennial screenings after three clean results reduced their anxiety and saved them time and money. "I still feel protected," they said. "It’s not about skipping care-it’s about smarter care."
Studies confirm both sides: when risk factors are ignored, progression happens fast. But when screening is tailored, outcomes improve dramatically. The UK’s national program, which uses risk stratification, has maintained a 99% success rate in preventing blindness over the last decade.

Barriers to Care and How to Overcome Them
Not everyone gets screened. In the U.S., only 58-65% of people with diabetes get annual eye exams. In rural areas, access is worse-22% of counties have no eye specialist within 50 miles. Cost is another barrier. In Australia, Medicare covers screening, but not all clinics offer it. Private insurance varies.
Solutions are emerging:
- Telemedicine: Remote image review cuts travel time and connects patients to specialists.
- Point-of-care devices: Tools like D-Eye let GPs do basic screenings during routine visits.
- AI-powered analysis: Reduces the need for human graders, speeding up results.
- Community outreach: Mobile screening units in low-income neighborhoods are showing promising results in reducing disparities.
Doctors are also getting better at explaining risk. Instead of saying, "Come back in a year," they now say, "Your risk is low because your HbA1c is stable. We can wait 2 years. But if it goes above 8%, we’ll need to see you sooner." That kind of clarity builds trust and compliance.
The Big Picture: Prevention Saves Sight
Diabetic retinopathy isn’t inevitable. It’s a signal-a warning that your diabetes needs tighter control. The same lifestyle changes that help your heart and kidneys also protect your eyes: eating well, moving daily, managing stress, and taking medications as prescribed.
By 2030, the World Health Organization estimates that widespread use of risk-based screening could prevent 2.5 million cases of blindness globally. That’s not just a statistic-it’s thousands of people keeping their jobs, driving their cars, reading to their kids, and living independently.
For you, it means one thing: don’t wait for symptoms. Get your eyes checked. Know your HbA1c. Ask your doctor: "What’s my risk? How often should I come back?" And if you’re told you can wait two years-make sure they’ve looked at your full picture, not just your last HbA1c.
Your vision isn’t something you can afford to gamble with. But with the right checks and care, you don’t have to.
How often should I get screened for diabetic retinopathy if I have type 2 diabetes and no eye damage?
If you have type 2 diabetes and no signs of retinopathy, and your HbA1c is below 7%, blood pressure is under 140/90, and you have no kidney disease, you can safely wait 2 to 4 years between screenings. Some people with very low risk may even go 5 years. But if your HbA1c is above 8% or you have high blood pressure, annual checks are still recommended.
Can diabetic retinopathy be reversed?
Early damage, like minor swelling or small vessel leaks, can improve with better blood sugar control and treatment like anti-VEGF injections. But once scar tissue forms or the retina detaches, the damage is permanent. That’s why early detection is everything-treatment stops progression, but it doesn’t restore lost vision.
Do I need to see an eye specialist, or can my GP do the screening?
Your GP can take retinal photos using tools like the D-Eye device, but they can’t diagnose or treat retinopathy. The images must be reviewed by a trained grader or ophthalmologist. In many cases, telemedicine services handle this remotely. You only need to see an eye specialist in person if screening shows moderate or worse retinopathy.
Are injections for diabetic macular edema painful?
The injections are done with numbing drops, so you feel pressure but little to no pain. Most people describe it as a brief sting or scratch. The whole process takes less than 10 minutes. Side effects are rare but can include temporary redness or floaters. Serious complications like infection happen in less than 1 in 1,000 cases.
If I get laser treatment, will I still need follow-ups?
Yes. Laser treatment doesn’t cure diabetic retinopathy-it only slows it down. You’ll still need regular eye checks, usually every 6 to 12 months, depending on your risk. The condition can progress even after treatment, especially if your blood sugar isn’t well controlled.
Is diabetic retinopathy screening covered by insurance in Australia?
Yes. Medicare covers full retinal photography screenings for people with diabetes at least once every two years. If you’re referred to an ophthalmologist for treatment, most procedures-including injections and laser therapy-are also covered. Some private health insurers offer additional benefits for advanced imaging or telehealth services.
If you’re managing diabetes, your eyes are just as important as your blood sugar numbers. Don’t let fear or convenience keep you from getting checked. The tools are here. The science is clear. And your sight? It’s worth protecting.


nikki yamashita
December 13, 2025 AT 09:41Adam Everitt
December 14, 2025 AT 13:17Reshma Sinha
December 15, 2025 AT 12:37Lawrence Armstrong
December 16, 2025 AT 04:30Audrey Crothers
December 17, 2025 AT 00:09Stacy Foster
December 17, 2025 AT 21:39Donna Anderson
December 19, 2025 AT 07:05sandeep sanigarapu
December 20, 2025 AT 21:57Ashley Skipp
December 22, 2025 AT 08:01Nathan Fatal
December 22, 2025 AT 20:01Robert Webb
December 23, 2025 AT 13:24wendy b
December 24, 2025 AT 13:18Rob Purvis
December 26, 2025 AT 03:45