DMD Progression Timeline Calculator
Progression Timeline
Explore typical milestones and symptom progression for Duchenne Muscular Dystrophy based on age and treatment options.
Early signs may include delayed motor milestones, difficulty running, or frequent falls. Diagnosis often occurs between ages 2-4 through genetic testing.
Typically diagnosed by age 5. Children may begin to use a wheelchair. Muscle weakness progresses, particularly in legs and pelvis. Physical therapy becomes essential.
Loss of ambulation often occurs between ages 6-12. Respiratory function begins to decline. Scoliosis may develop. Physical therapy helps maintain joint flexibility and prevent contractures.
Respiratory decline accelerates. Ventilator support may be needed. Cardiac issues may emerge. Cognitive development may be affected in some cases.
Respiratory and cardiac complications become more significant. Long-term management focuses on quality of life. Early treatment options may slow disease progression.
Key Milestones
Diagnosis Age
Typically occurs between ages 2-4 through genetic testing
Loss of Ambulation
Most commonly between ages 6-12
Respiratory Decline
Often begins in teenage years
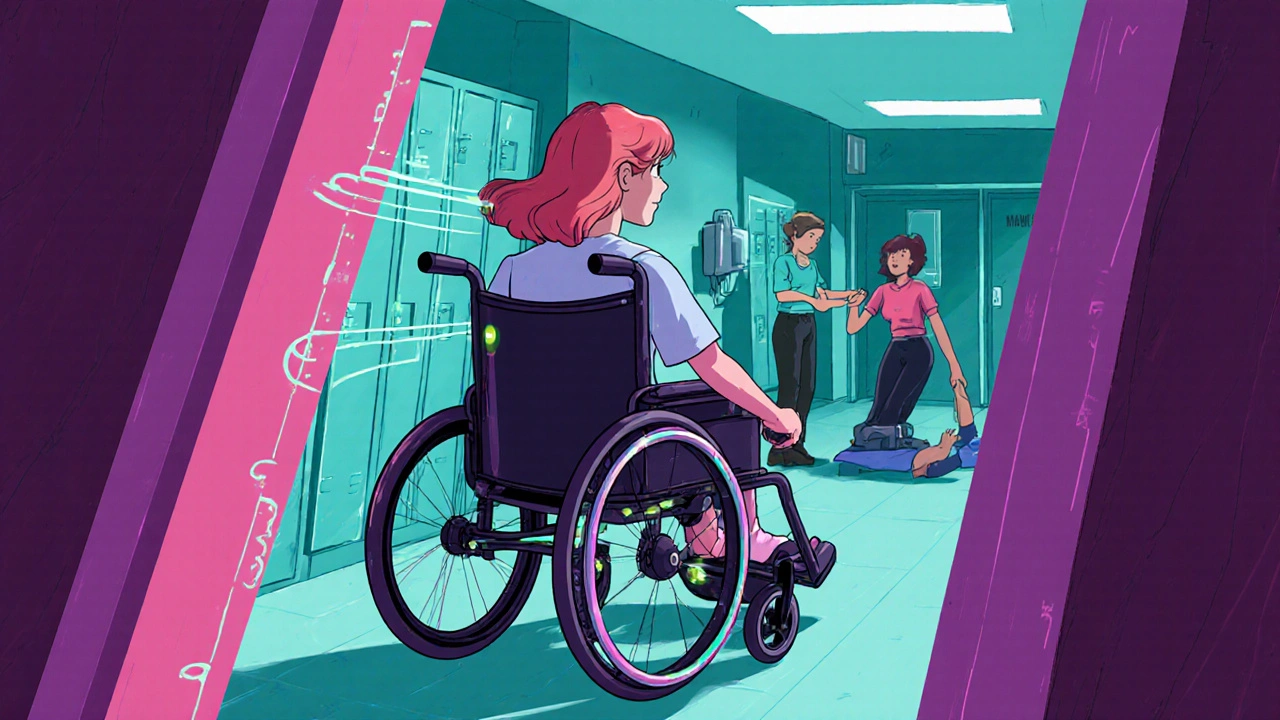
Living with Duchenne Muscular Dystrophy is a daily test of courage, but the community shows how hope turns into action.
What is Duchenne Muscular Dystrophy?
Gene therapy is often mentioned alongside the disease, but first let’s break down the basics. Duchenne Muscular Dystrophy (DMD) is a genetic disorder caused by mutations in the dystrophin gene. The missing protein leads to progressive muscle weakness, usually appearing before age five.
The condition affects about 1 in 3,500 male births worldwide. Because the gene is on the X‑chromosome, girls are typically carriers and rarely show symptoms.
Daily Life Challenges Faced by People with DMD
From the moment a child learns to crawl, families confront a steep learning curve. Simple tasks like climbing stairs or holding a pencil become hurdles. Physical therapy helps maintain joint flexibility, but therapy sessions can feel endless.
Respiratory decline often starts in the teenage years, making Ventilator support a reality for many. Schools must adapt curricula, and workplaces need accessible equipment.
Inspiring Community Stories
Below are three snapshots of real people who have turned challenges into milestones.
- Alex, 22, college student: After a clinical trial, Alex received a one‑time Gene therapy infusion. While not a cure, the treatment slowed muscle loss, allowing him to graduate with a degree in graphic design.
- Mia, 15, high‑school athlete: Mia uses a custom‑fit Assistive technology wheelchair that tracks her posture in real time. The device alerts her parents when she shifts weight for too long, preventing contractures.
- James, 38, caregiver: James’s younger sister is a DMD carrier. He coordinates home Corticosteroids schedules, physical therapy appointments, and school meetings, turning chaos into a manageable routine.
Practical Coping Strategies
Here are tips that the community repeatedly mentions as game‑changers.
- Build a dedicated medical calendar. Online tools can send reminders for medication refills, therapy sessions, and doctor visits.
- Engage with a multidisciplinary team: neurologist, pulmonologist, physiotherapist, and a social worker who understands insurance hurdles.
- Choose the right Assistive technology early. An ergonomic seating system can prevent scoliosis later.
- Stay informed about ongoing Clinical trials. Registries like ClinicalTrials.gov list studies recruiting worldwide.
- Connect with support groups-both in‑person and online. Sharing stories reduces isolation and surfaces creative solutions.
Emerging Treatments Offering Hope
Beyond the traditional Corticosteroids, several new avenues are gaining traction.
| Therapy | Mechanism | Stage | Key Benefit |
|---|---|---|---|
| Exon Skipping | Restores reading frame | Phase 3 | Improves walking speed |
| Gene Therapy (Micro‑dystrophin) | Delivers functional dystrophin | Phase 2/3 | Slows overall decline |
| Utrophin Up‑regulation | Boosts compensatory protein | Pre‑clinical | Potential long‑term muscle preservation |
While each option has its own risk profile, families report that even incremental gains translate into more school days, extra time with friends, and a better quality of life.
Tips for Caregivers
Caregivers often shoulder the emotional weight of appointments and the practical side of daily care. Here are three proven habits:
- Self‑care scheduling: Allocate at least one hour a week for exercise, meditation, or a hobby-burnout reduces the quality of care you can give.
- Financial planning: Early conversations with a financial advisor can set up a Special Needs Trust, protecting assets for the future.
- Education advocacy: Learn your child’s rights under the Individuals with Disabilities Education Act (IDEA). A well‑crafted Individualized Education Program (IEP) can secure needed accommodations.

Building a Support Network
The DMD community thrives on connection. Social media platforms like Facebook and Reddit host active groups where families share equipment reviews, trial updates, and emotional support. Local chapters of the Muscular Dystrophy Association (MDA) organize fundraising runs that double as awareness events.
When you feel isolated, remember that reaching out is a strength, not a weakness. A single conversation can spark a partnership that eases transportation, shares therapy tips, or simply offers a listening ear.
Living with Hope
Every story highlighted here underscores a common thread: resilience fueled by community. Whether it’s a breakthrough Duchenne muscular dystrophy treatment or a simple weekend outing, the small victories add up to a meaningful life.
Frequently Asked Questions
What age is DMD usually diagnosed?
Most boys show signs before age five, and a definitive diagnosis often follows genetic testing between ages 2 and 4.
Can gene therapy cure DMD?
Current gene‑therapy approaches aim to slow disease progression rather than cure it. Ongoing trials are evaluating long‑term safety and effectiveness.
How does physical therapy help?
Regular stretching and low‑impact exercises preserve joint range of motion, delay contractures, and support breathing muscles.
What financial resources are available?
The Muscular Dystrophy Association, state disability programs, and Special Needs Trusts can offset medical costs and equipment expenses.
Where can I find clinical trials?
Websites like ClinicalTrials.gov and the MDA’s research portal list active DMD trials worldwide.


Darryl Gates
October 17, 2025 AT 13:34Hey everyone, great compilation of resources! Keeping a medical calendar and a multidisciplinary team really makes the day‑to‑day less chaotic. Remember to celebrate even the smallest functional gains-they add up over time. Stay strong and keep supporting each other.
Winston Bar
October 18, 2025 AT 11:48Sure, gene therapy is the magic bullet-if you believe fairy tales.
Russell Abelido
October 19, 2025 AT 10:01The journey with Duchenne feels like navigating a foggy sea where each lighthouse is a breakthrough. When we read about exon skipping, we glimpse a beacon that promises to restore a sliver of lost function. Yet the path is littered with clinical trial hoops, insurance mazes, and the quiet grief of unmet expectations. It is in those moments that community stories become the compass that points us forward. Alex’s graduation, for example, illustrates how a single infusion can shift the trajectory enough to finish a degree. Mia’s adaptive wheelchair shows that technology can become an ally, not just a gadget. James’s caregiving routine reminds us that organization is a form of love, a silent heroics behind every appointment. The small victories, like a new stretch routine that eases contractures, deserve applause as loudly as a medical milestone. Your tip about a dedicated calendar may seem simple, but it is a lifeline that prevents missed doses and rushed visits. I have seen families who missed a corticosteroid refill and faced a setback that could have been avoided with a reminder. The emotional weight of coordinating care can be overwhelming, but sharing those stories lightens the load for newcomers. Remember, resilience isn’t a solo sport; it’s a relay where each participant hands over hope to the next. Embracing multidisciplinary teams means you get a neurologist’s expertise, a pulmonologist’s vigilance, a physiotherapist’s guidance, and a social worker’s advocacy-all dancing together in harmony. When you stay informed about trial registries, you become a proactive player rather than a passive observer. Keep the conversation alive, celebrate each step, and let the community’s collective spirit lift you up 🙂.
Steve Holmes
October 20, 2025 AT 08:14Wow, this post packs a lot of useful info, and I love how each section flows, from genetics to practical tips, and the layout makes it easy to skim, yet deep enough to dig in, especially the table comparing emerging therapies, which is a fantastic quick reference, plus the bullet points on caregiver self‑care are gold, keep it coming!
Roberta Makaravage
October 21, 2025 AT 06:28Honestly, anyone who dismisses the importance of a Special Needs Trust is ignoring basic financial ethics 🙅♀️. The article correctly emphasizes planning early, because the moral responsibility to protect a child’s future cannot be understated 💡. Also, the community’s push for accessible education aligns with the universal principle of equity 📚. Let’s all champion these proven strategies! 🚀
Malia Rivera
October 22, 2025 AT 04:41One could argue that focusing on gene therapy distracts from the everyday battles families face, yet the science does not exist in a vacuum, so we must balance hope with realistic expectations, and perhaps the true philosophy is to use every tool while never forgetting the human element.
Kate Marr
October 23, 2025 AT 02:54Our nation's commitment to research should translate into funding for schools that adapt curricula for DMD students, and that’s why I’m cheering every grant awarded 🇺🇸💪.
James Falcone
October 24, 2025 AT 01:08Just saying, the community’s hustle is what keeps the fight alive, and that’s something we should all respect.
Frank Diaz
October 24, 2025 AT 23:21The article’s optimism feels a bit glossy when the lived reality includes insurance denials, chronic pain, and emotional fatigue. A philosophical lens reveals that hope can become a veil that obscures systemic flaws. It’s critical to interrogate why access to cutting‑edge therapies remains uneven. Only then can we claim true progress.
Mary Davies
October 25, 2025 AT 21:34The drama of daily life with DMD is a silent opera, each breath a note, each therapy session a chorus. When we talk about “incremental gains,” we’re really describing humanity’s stubborn refusal to surrender. The story of Alex graduating is not just a personal triumph; it’s a testament to collective perseverance. Caregivers, remember that your self‑care moments are not selfish-they’re essential interludes that sustain the performance. Let the music play on.
Carissa Padilha
October 26, 2025 AT 18:48There’s a hidden agenda behind the glossy press releases on gene therapy, and it’s not just about scientific curiosity. Some think the “clinical trials” are a distraction from the real power structures that benefit from keeping families dependent. Think about the data that never gets published, the side effects that are swept under carpet. It feels like a coordinated narrative to sell hope, not cure. Keep your eyes open; the truth is often buried in plain sight.
Richard O'Callaghan
October 27, 2025 AT 17:01Honestly i think the post is great but i cant help but wonder why no mention of mental health resources, it’s kinda an oversight. Also, the table could use more colors to make it easier on the eyes. Lets not forget that support groups also need funding.